Healing From Within: Are Mesenchymal Stem Cells the Future for Rotator Cuff Repairs

Shoulder pain is more than just an inconvenience. For those suffering from a rotator cuff tear, it can mean the end of a fitness routine, difficulty sleeping, or persistent pain during simple daily tasks such as reaching for a shelf or lifting light objects.
Traditional treatment options typically range from conservative physical therapy to invasive surgical repair. While these approaches can be effective, a promising frontier in regenerative medicine is gaining momentum: Mesenchymal Stem Cell (MSC) therapy. This biologic approach focuses on healing damaged tissue rather than merely repairing it mechanically.
The rotator cuff is a group of four muscles and tendons responsible for stabilizing the shoulder joint. Because tendons have a relatively poor blood supply compared to muscle tissue, they heal slowly and incompletely. Even after surgical repair, failure-to-heal rates remain significant, as the body often replaces healthy tendon tissue with stiff, weakened scar tissue.
Mesenchymal Stem Cells are multipotent cells typically harvested from a patient’s own bone marrow or adipose (fat) tissue. Their value in shoulder injuries lies not only in their ability to become new tissue, but also in their role as biological managers within the healing environment.
When injected into a damaged rotator cuff, MSCs act through three primary mechanisms. First, they reduce inflammation by releasing signaling molecules that calm chronically irritated tissue. Second, they recruit additional healing cells to migrate to the injury site. Third, they promote the formation of organized, healthy collagen rather than dysfunctional scar tissue.

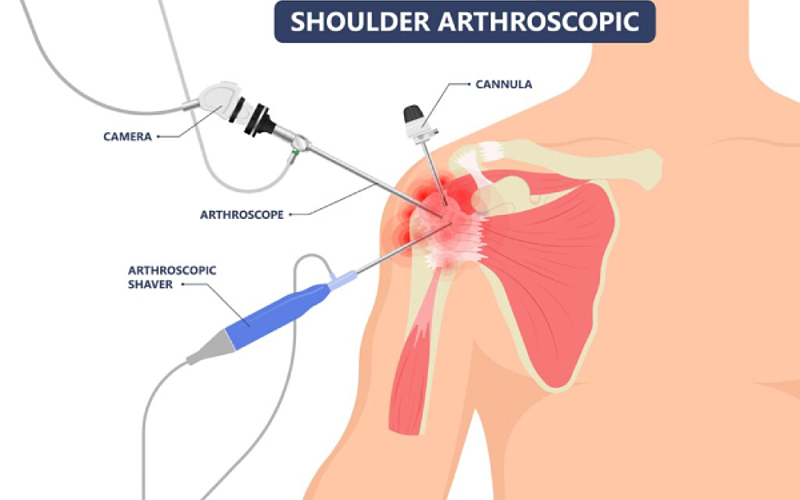
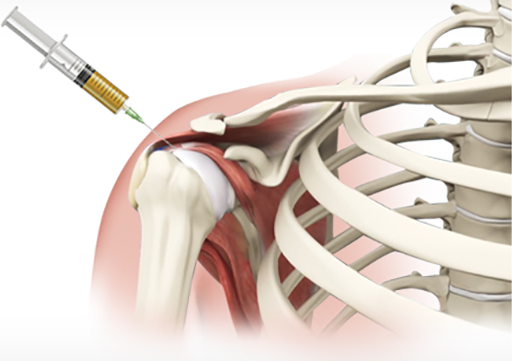
Unlike surgery, MSC therapy is usually performed as a minimally invasive outpatient procedure. Cells are extracted under local anesthesia, processed through centrifugation to concentrate regenerative components, and then injected directly into the injured area using ultrasound guidance for precision.
MSC therapy is commonly considered for patients with partial tears or chronic tendinopathy who have not responded adequately to physical therapy. It is also increasingly used as an adjunct during surgical repair to help strengthen tendon-to-bone healing and reduce retear risk.
While research is ongoing and results may vary based on injury severity and patient-specific factors, the goal remains consistent: reduced pain, improved function, and faster recovery. For patients seeking alternatives to prolonged surgical downtime, regenerative medicine may offer a meaningful path forward.
Importantly, patient selection and clinical oversight matter greatly. Outcomes depend on imaging accuracy, injection technique, cell dose, rehabilitation compliance, and realistic expectations. When combined with guided physical therapy and lifestyle adjustments, regenerative approaches may complement—not replace—sound orthopedic care, offering another option for patients seeking durability, safety, and function across diverse ages, activity levels, and tear patterns worldwide today forward.
Final Thought: If you’re looking to avoid the extended downtime of surgery—or are dealing with a tear that just won’t heal—regenerative medicine may provide the biologic boost your shoulder needs.
Disclaimer: This content is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare provider.
‹ Back